Showing posts with label snippet. Show all posts
Showing posts with label snippet. Show all posts
Wednesday, May 4, 2011
Pantoprazole infusion
For actively bleeding ulcers give pantoprazole bolus followed by infusion.
- LOading dose: Pantoprazole 80mg IV in 100ml of NaCl 0.9% or 5% glucose over 20 - 30 minutes
- Infusion:
- Pantoprazole 200mg in Dextrose 5% 500mL at 20mL/hr (each mL is 0.4mg , 20mL/hr = 8mg/hr, 1mg =2.5mL)
- Pantoprazole 80mg in N/Saline 100mL at 10mL/hr (each mL is 0.8mg , 10mL/hr = 8mg/hr,1mg=1.25mL)
References
Tuesday, January 25, 2011
Blood Gas normal values
| Arterial | Venous | |
| pH | 7.35-7.45 | 7.3-7.35 |
| pCO2 | 35-45 | 45-46 (good representation of ventilation) |
| pO2 | 80-100 | 20-80 (uninterprable) |
| SaO2 | 95-100 | |
| HCO3- | 22-28 | |
| BE | +/- 3 |
Labels:
ED,
ICU,
medicine,
physiology,
Respiratory,
snippet
Sunday, May 9, 2010
AMIs and thrombolysis
ECG changes indicating AMI
- High probability of MI: persistent ST elevation of ≥ 1 mm in two contiguous limb leads or ST-segment elevation of ≥ 2 mm in two contiguous chest leads or the presence of new LBBB.
- Intermediate probability of MI: are ST depression, T-wave inversion, and other nonspecific ST-T wave abnormalities.
- Q waves = old MI
DDxes
- Aortic dissection
- Pericarditis (would show on all leads)
- Pulmonary embolism
Management options
- Patients with persistent ST elevation should be considered for reperfusion therapy (thrombolysis or primary PCI).
- Those without ST elevation will be diagnosed with either NSTEMI if cardiac marker levels are elevated or with unstable angina if serum cardiac marker levels provide no evidence of myocardial injury. Patients presenting with no ST-segment elevation are not candidates for immediate thrombolytics but should receive anti-ischemic therapy and may be candidates for PCI urgently or during admission.
Medical Management
- Aspirin (300 mg) should be given unless already taken or contraindicated (grade A recommendation), and should preferably be given early (eg, by emergency or ambulance personnel).
- Clopidogrel should be given in addition to aspirin for patients undergoing PCI with a stent (loading-dose of 300–600 mg), or for fibrinolytic therapy (300 mg). Clopidogrel 75 mg daily should be continued for at least a month after fibrinolytic therapy, and for up to 12 months after stent implantation, depending on the type of stent.
- Antithrombin therapy to inhibit the coagulation cascade, and for patients underdoing PCI. For patients getting streptokinase, whether to heparinise depends on the anti-thrombotic agent. Clexane (enoxaparin) bolus should be dosed at 0.75 mg/kg.
- Administer a platelet glycoprotein (GP) IIb/IIIa-receptor antagonist (eptifibatide, tirofiban, or abciximab) in addition to aspirin and unfractionated heparin, to patients with continuing ischemia or with other high-risk features and to patients in whom PCI is planned.
- An ACE inhibitor (Captopril) should be given orally within the first 24 hours of STEMI to patients with anterior infarction, pulmonary congestion, or left ventricular ejection fraction (LVEF) less than 40% in the absence of hypotension.
- An angiotensin receptor blocker (valsartan or candesartan) should be administered to patients with STEMI who are intolerant of ACE inhibitors and who have either clinical or radiological signs of heart failure or LVEF less than 40%.
Contraindications for fibrinolytic use in STEMI
Absolute contraindications:- Prior intracranial hemorrhage (ICH)
- Known structural cerebral vascular lesion
- Known malignant intracranial neoplasm
- Ischemic stroke within 3 months
- Suspected aortic dissection
- Active bleeding or bleeding diathesis (excluding menses)
- Significant closed-head trauma or facial trauma within 3 months
- History of chronic, severe, poorly controlled hypertension
- Severe uncontrolled hypertension on presentation (SBP >180 mm Hg or DBP >110 mm Hg)
- Traumatic or prolonged (>10 min) CPR or major surgery less than 3 weeks
- Recent (within 2-4 wk) internal bleeding
- Noncompressible vascular punctures
- For streptokinase/anistreplase - prior exposure or prior allergic reaction to these agents
- Pregnancy
- Active peptic ulcer
- Current use of anticoagulant (eg, warfarin sodium) that has produced an elevated international normalized ratio (INR) >1.7 or prothrombin time (PT) >15 seconds
Follow-up Patient Care
- Patients should continue to receive beta-blockers, nitrates, and heparin, as indicated.
- ACE inhibitors have been shown to improve survival rates in patients who have experienced an MI. In the acute setting, afterload reduction from ACE inhibitors may reduce the risk of CHF and sudden death.
References
Friday, March 12, 2010
Guardianship
If a patient refuses treatment...
- If NOK agrees not to treat → OK but document it
- If NOK thinks treatment should occur → need to go to guardianship tribunal
Sunday, January 17, 2010
Antibodies
Antibodies consist of two Ig heavy chains (blue) linked by disulfide bonds to two Ig light chains (green).
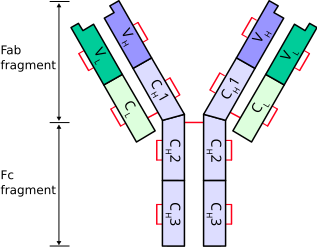
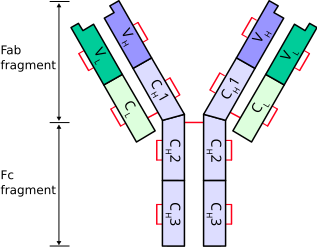
Heavy chains
Heavy chains define the class of immunoglobulin. There are 5 types of heavy chains:- α (Ig A)
- δ (Ig D)
- ε (Ig E)
- γ (Ig G)
- μ (Ig M)
Light chains
There are 2 types of light chains:- Lambda (λ) - encoded by a gene on chromosome 22
- Kappa (κ) - encoded by a gene on chromosome 2
References
- http://en.wikipedia.org/wiki/Immunoglobulin_heavy_chain
- http://en.wikipedia.org/wiki/Immunoglobulin_light_chain
- http://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology
- http://www3.interscience.wiley.com/journal/120047597/abstract?CRETRY=1&SRETRY=0
Labels:
haematology,
pathology,
physiology,
snippet
Friday, January 15, 2010
Well’s Criteria for DVT
The Score
- Active cancer (treatment within last 6 months or palliative) -- 1 point
- Calf swelling >3 cm compared to other calf (measured 10 cm below tibial tuberosity) -- 1 point
- Collateral superficial veins (non-varicose) -- 1 point
- Pitting edema (confined to symptomatic leg) -- 1 point
- Swelling of entire leg - 1 point
- Localized pain along distribution of deep venous system—1 point
- Paralysis, paresis, or recent cast immobilization of lower extremities—1 point
- Recently bedridden > 3 days, or major surgery requiring regional or general anesthetic in past 4 weeks—1 point
- Alternative diagnosis at least as likely—Subtract 2 points
Interpretation
Score of 2 or higher - deep vein thrombosis is likely. Consider imaging the leg veins.Score of less than 2 - deep vein thrombosis is unlikely. Consider blood test such as d-dimer test to further rule out deep vein thrombosis.
References
- http://en.wikipedia.org/wiki/Deep_vein_thrombosis
- http://emedicine.medscape.com/article/758140-overview
Tuesday, January 12, 2010
CHAD2 (CHADS) score
The CHADS score is a clinical prediction rule for estimating the risk of stroke in patients with non-rheumatic atrial fibrillation (AF) and is used to determine the degree of anticoagulation therapy required.
H ypertension > 160mmHg systolic (or treated hypertension) (1 point)
A ge > 75 (1 point)
D iabetes (1 point)
S - previous stroke or TIA (2 points)

To Score...
C ongestive heart failure (1 point)H ypertension > 160mmHg systolic (or treated hypertension) (1 point)
A ge > 75 (1 point)
D iabetes (1 point)
S - previous stroke or TIA (2 points)
Risk of stroke based on CHADS score

Recommendations for anticoagulation
- High risk (score >= 2) - warfarin (unless contrainidcated)
- Moderate risk (score 1) - aspirin or warfarin
- Low risk (score 0) - aspirin
References
- http://en.wikipedia.org/wiki/CHADS_Score
- http://www.cardiology.org/tools/risk_of_stroke_AF.html
Friday, January 8, 2010
ABCD^2 (ABCD squared) post TIA stroke risk assessment tool
The Tool
AGE: greater than or equal to 60 years – 1 pointBlood Pressure: Systolic >= 140, diastolic >= 90 (when first assessed after TIA) – 1 point
Clinical Features: unilateral weakness – 2 points, isolated speech disturbance – 1 point, other – zero
Duration of TIA symptoms: greater than or equal to 60 minutes – 2 points, 10 to 59 minutes – 1 point, <10 minutes zero
Diabetes present – 1 point
Estimated two day stroke risks determined by the ABCD^2 score:
- Score 6 to 7: High two day stroke risk (8.1%)
- Score 4 to 5: Moderate two day stroke risk (4.1%)
- Score 0 to 3: Low two day stroke risk (1.0%)
- Score < 1: Very low two day stroke risk (0.0%)
In versus outapatient management
People with a high risk of stroke (ABCD2 score of 4 or above) should have:- Aspirin (300 mg daily) started immediately
- specialist assessment and investigation within 24 hours of onset of symptoms
- measures for secondary prevention introduced as soon as the diagnosis is confirmed, including discussion of individual risk factors
- Aspirin (300 mg daily) started immediately
- specialist assessment and investigation as soon as possible, but definitely within 1 week of onset of symptoms
- measures for secondary prevention introduced as soon as the diagnosis is confirmed, including discussion of individual risk factors
Investigations
- CT scan without enhancement should be done in all patients to exclude other causes of neurological deficit (e.g. hemorrhage, subdural hematoma)
- The presence of an infarct on CT is highly predictive of subsequent stroke
- Early CT showing hemorrhage makes carotid imaging unnecessary
- Carotid imaging should be done for all patients with symptoms in anterior circulation territory.
- The presence of carotid disease is highly predictive of recurrent stroke.
- Consider CT angiogram if Carotid Ultrasound cannot be obtained in reasonable time.
- ECG and occasionally Holter monitoring to detect atrial fibrillation.
- ECHO cardiogram for persons with suspect underlying cardiac abnormalities.
- Blood sugar to detect extremes in glucose levels.
References
- http://bmhgt.com/2009/03/stroke-information-abcd2/
- http://www.gpnotebook.co.uk/simplepage.cfm?ID=x20080723164438749131
- http://www.palmedpage.com/Text_files/Neurology/ABCD/TIA%20Management.html
- http://www.stroke.org/site/DocServer/NSA_ABCD2_tool.pdf?docID=5981
Wednesday, November 18, 2009
Sedation tips
- Don't use midazolam and olanzapine together as it can cause rapid onset respiratory depression. Clonazepam and olanzipine is a better combination.
- Chlorpromazine is also good. Non-addictive, and comes as a liquid.
Labels:
medicine,
pharmacology,
psychiatry,
snippet
Wednesday, November 4, 2009
Blood Products timing
RBCs 1 unit q4h
FFP 1 unit q1h
Platelets 1 unit q30minutes
FFP 1 unit q1h
Platelets 1 unit q30minutes
Labels:
haematology,
IVfluids,
management,
medicine,
pathology,
snippet
Thursday, September 17, 2009
Tuesday, September 15, 2009
Home Oxygen
Criteria to qualify:
- pO2 < 55
- SaO2 < 90% RA
- Non-smoker!
Labels:
asthma,
GenMed,
medicine,
Respiratory,
snippet
Friday, September 11, 2009
Saturday, August 22, 2009
Peutz–Jeghers syndrome
- Peutz–Jeghers syndrome is also known as hereditary intestinal polyposis syndrome.
- An autosomal dominant genetic disease characterized by the development of benign hamartomatous polyps in the GIT and hyperpigmented macules on the lips and oral mucosa.
- Prevalence of approximately 1 in 100,000 to 200,000 births.
Diagnosis
Need 2 of 3 of:- Family history
- Mucocutaneous lesions causing patches of hyperpigmentation in the mouth and on the hands and feet.
- Oral pigmentations are the first to appear and play an important part in early diagnosis. Intraorally, they are most frequently seen on the gingiva, hard palate and inside of the cheek. The mucosa of the lower lip is almost invariably involved as well.
- Hamartomatous polyps in the gastrointestinal tract. These are benign polyps with an extraordinarily low potential for malignancy.
- Mutation in the tumour supressor gene STK11 on chromosome 19.
Natural history
- Most patients will develop melanotic macules during the first year of life.
- Intussusception usually first occurs between the ages of six and 18 years old.
- Most people will have developed some form of neoplastic disease by age 60.
- Cumulative lifetime cancer risk begins to rise in middle age.
- Cumulative risks by age 70 for all cancers, gastrointestinal (GI) cancers, and pancreatic cancer are 85%, 57%, and 11%, respectively.
References
- http://en.wikipedia.org/wiki/Peutz-Jeghers_syndrome
- http://www.answers.com/topic/peutz-jeghers-syndrome
Tuesday, August 28, 2007
Microalbumuria
Screening for microalbumuria in non-diabetics is a good way to screen for CV risks. The microalbumuria is caused by endothelial dysfunction.
Electrolyte imbalances that occur in diabetes
- Hypocalcaemia - kidney doesn't activate vitamin D -> decreased GIT absorption of Ca
- Hyponatraemia
- Hyperphosphataemia - it can't be excreted. Treatment is by giving a phosphate binder e.g. mylanta.
Labels:
diabetes,
electrolytes,
endocrine,
snippet
Treatment of endocarditis
Endocarditis requires 6 weeks of IV antibiotic treatment. This length of time is required because it is difficult for antibiotics to penetrate to the valve cusps which are relatively avascular.
Labels:
antibiotics,
CV,
management,
snippet
Thursday, August 23, 2007
Calcium channel blockers
Mechanism of action
Calcium channel blockers have a negative inotropic effect - they decrease the force of contraction of the myocardium.They block L-type voltage gated calcium channels in the heart and blood vessels. This prevents calcium levels from increasing as much in the cells when stimulated, leading to less contraction.
They also decrease total peripheral resistance by dilating the blood vessels, and decreasing cardiac output by lowering the force of contraction. Because resistance and output drop, so does blood pressure. With low blood pressure, the heart does not have to work as hard; this can ease problems with cardiomyopathy and coronary disease.
Unlike with beta-blockers, the heart is still responsive to sympathetic nervous system stimulation, so blood pressure can be maintained more effectively.
Many calcium channel blockers also slow down the conduction of electrical activity within the heart by blocking the calcium channel during the plateau phase of the action potential of the heart. This causes a lowering of the heart rate and may cause heart blocks (negative chronotropic effect) of calcium channel blockers.
Classes
There are 2 classes of CCBs:- Dihydropyridines
- Used to reduce systemic vascular resistance and arterial pressure, but are not used to treat angina because the vasodilation and hypotension can lead to reflex tachycardia.
- This CCB class is easily identified by the suffix "-pine" e.g. Amlodepine, Felodipine.
- Used to reduce systemic vascular resistance and arterial pressure, but are not used to treat angina because the vasodilation and hypotension can lead to reflex tachycardia.
- Non-dihydropyridines
- Relatively selective for myocardium, reduce myocardial oxygen demand and reverse coronary vasospasm, and are often used to treat angina.
- They have minimal vasodilatory effects compared with dihydropyridines.
- Action is intracellular.
- E.g. verapamil.
- Relatively selective for myocardium, reduce myocardial oxygen demand and reverse coronary vasospasm, and are often used to treat angina.
Indications
- Atrial fibrillation or flutter - to control heart rate via negative chronotropic effect.
Contraindications
- Avoided (or used with caution) in individuals with cardiomyopathy due to negative inotropic effect.
- Non-dihydropyridine CCBs should not be combined with beta-blockers because they are both negative inotropes and affect the AV node.
- Wikpedia, http://en.wikipedia.org/wiki/Calcium_channel_blocker
Subscribe to:
Posts (Atom)
