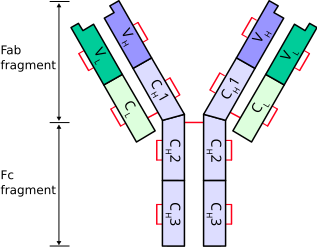
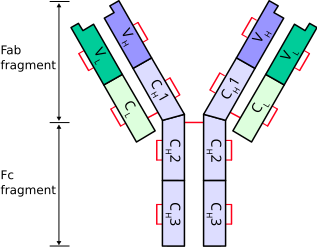
Antibodies consist of
two Ig heavy chains (blue) linked by disulfide bonds to
two Ig light chains (green).
Heavy chains
Heavy chains define the
class of immunoglobulin. There are 5 types of heavy chains:
- α (Ig A)
- δ (Ig D)
- ε (Ig E)
- γ (Ig G)
- μ (Ig M)
The immunoglobulin heavy chain gene complex has been assigned to
chromosome 14.
Light chains
There are 2 types of light chains:
- Lambda (λ) - encoded by a gene on chromosome 22
- Kappa (κ) - encoded by a gene on chromosome 2
Ig light chains produced in neoplastic plasma cells (e.g. in multiple myeloma) are called
Bence Jones proteins.
References
- http://en.wikipedia.org/wiki/Immunoglobulin_heavy_chain
- http://en.wikipedia.org/wiki/Immunoglobulin_light_chain
- http://en.wikipedia.org/wiki/Multiple_myeloma#Pathophysiology
- http://www3.interscience.wiley.com/journal/120047597/abstract?CRETRY=1&SRETRY=0